Digestive health topics are trending more than ever, and many people are searching online for answers about what does poop look like with diverticulitis. Stomach pain, changes in bowel habits, and unusual stool appearance can be worrying. Because diverticulitis affects the digestive tract, it often changes how bowel movements look and feel.
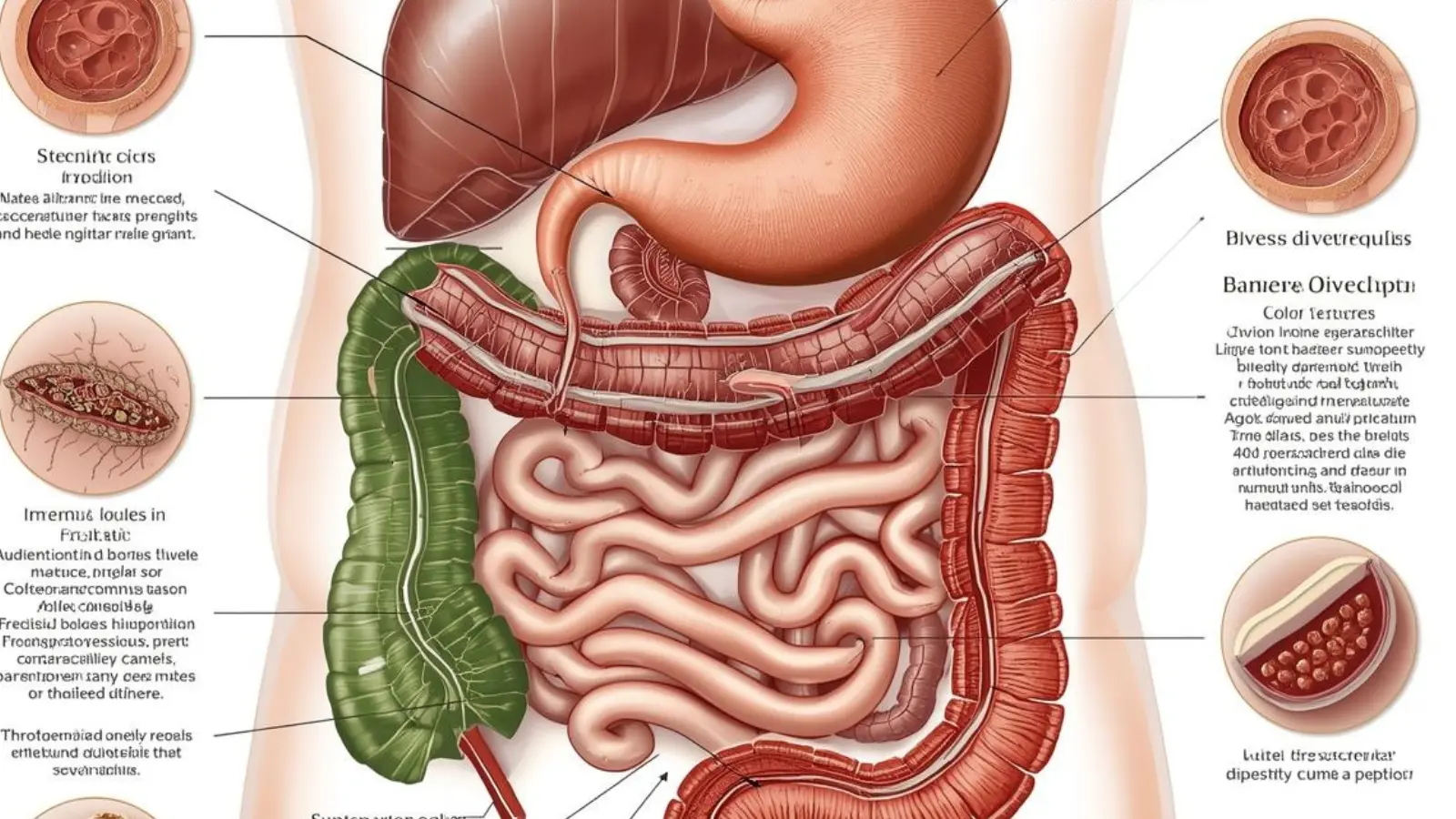
Diverticulitis is a condition where small pouches (called diverticula) in the colon become inflamed or infected. When this happens, stool appearance can change in color, shape, consistency, and even smell. Understanding these changes can help you know when to seek medical attention.
⚡ Quick Answer
Poop with diverticulitis may look thinner than usual, loose or watery, dark, or even contain mucus or blood. Some people also experience constipation with small, hard stools.
Understanding Diverticulitis and Bowel Changes
Before looking at stool appearance in detail, it’s important to understand what diverticulitis does to the body.
The colon (large intestine) forms small bulging pouches in some people, especially after age 40. This condition is called diverticulosis. When those pouches become inflamed or infected, it turns into diverticulitis.
Because the colon’s main job is to form stool, any inflammation can affect:
- Stool shape
- Stool color
- Stool texture
- Frequency of bowel movements
- Presence of mucus or blood
What Does Poop Look Like With Diverticulitis?
Below are the most common changes people notice.
1. Thin or Pencil-Shaped Stool
Inflammation can narrow part of the colon. When that happens, stool may come out:
- Thin
- Narrow
- Ribbon-like
If thin stool continues for several days along with pain or fever, medical advice is important.
2. Loose or Watery Stool (Diarrhea)
Some people experience:
- Frequent loose bowel movements
- Urgent need to go
- Mild to severe diarrhea
This happens because inflammation irritates the colon lining.
3. Hard, Small, or Lumpy Stool (Constipation)
Others may have the opposite problem:
- Hard pellets
- Small, difficult-to-pass stool
- Feeling like you didn’t fully empty your bowels
Constipation can increase pressure in the colon, worsening symptoms.
4. Mucus in Stool
Inflamed intestines may produce extra mucus. You might notice:
- Slimy coating on stool
- Clear or white jelly-like substance
Small amounts of mucus can happen normally, but frequent mucus may signal irritation.
5. Blood in Stool
This can appear as:
- Bright red streaks
- Dark red clots
- Black, tar-like stool (if bleeding is higher up)
Blood in stool should always be checked by a doctor.
6. Foul-Smelling Stool
Infection may cause:
- Stronger-than-usual odor
- Unusual smell that persists
This is due to bacterial imbalance and inflammation.
Stool Color Changes in Diverticulitis
Here’s a simple table to understand possible stool color changes:
| Stool Color | Possible Meaning |
|---|---|
| Brown | Normal |
| Yellow | Mild digestive issue |
| Green | Fast digestion |
| Red | Possible bleeding |
| Black | Upper digestive bleeding |
| Pale | Bile flow issue |
If stool is red or black, seek medical help immediately.
Other Symptoms That Happen With Stool Changes
Stool appearance is only part of the picture. Diverticulitis often includes:
- Lower left abdominal pain
- Fever
- Nausea
- Bloating
- Loss of appetite
- Fatigue
If these symptoms occur together with unusual stool, medical care may be needed.
When to See a Doctor
Contact a healthcare provider if you notice:
- Blood in stool
- Severe abdominal pain
- High fever
- Ongoing diarrhea or constipation
- Vomiting
- Dizziness
Early treatment prevents complications like abscess or bowel rupture.
Mild vs Severe Diverticulitis
Mild Cases
- Slight stool changes
- Mild pain
- Low-grade fever
Often treated with rest and dietary changes.
Severe Cases
- Significant bleeding
- Severe pain
- High fever
- Persistent bowel changes
May require antibiotics or hospital care.
How Diet Affects Stool in Diverticulitis
During a flare-up, doctors may recommend:
Clear Liquid Diet (Short-Term)
- Broth
- Water
- Clear juices
- Gelatin
This helps the colon rest.
Low-Fiber Diet (During Recovery)
- White rice
- White bread
- Eggs
- Cooked vegetables
High-Fiber Diet (Prevention Phase)
Once healed, fiber helps prevent future flare-ups:
- Whole grains
- Fruits
- Vegetables
- Beans
Always increase fiber gradually.
How to Monitor Your Stool Safely
It may feel uncomfortable to observe bowel movements, but it helps detect problems early.
Look for:
- Shape
- Color
- Consistency
- Presence of mucus
- Presence of blood
You can use the Bristol Stool Chart as a guide:
- Type 1–2: Constipation
- Type 3–4: Normal
- Type 5–7: Diarrhea
Is It Always Diverticulitis?
Other conditions can cause similar stool changes:
- Irritable Bowel Syndrome (IBS)
- Hemorrhoids
- Colon polyps
- Colorectal cancer
- Infections
That’s why proper medical evaluation is important.
Frequently Asked Questions (FAQ)
What does poop look like with diverticulitis really mean?
It refers to changes in stool appearance caused by inflammation in the colon. These changes may include thin stool, mucus, blood, diarrhea, or constipation.
Is blood in stool common with diverticulitis?
It can happen, but it’s not always present. Any blood in stool should be checked by a healthcare provider.
Is diverticulitis stool always diarrhea?
No. Some people experience diarrhea, while others have constipation. It varies from person to person.
Can stool return to normal after treatment?
Yes. With proper treatment and healing, bowel movements usually return to normal.
How should someone respond if they notice changes?
If stool changes last more than a few days or include pain or fever, schedule a medical appointment.
Key Takeaways
- Diverticulitis can change stool shape, color, and consistency.
- Thin, watery, hard, or mucus-covered stool may occur.
- Blood in stool requires immediate medical attention.
- Stool changes often come with abdominal pain and fever.
- Early treatment prevents serious complications.
Conclusion
Understanding what does poop look like with diverticulitis helps you recognize warning signs early. Stool may become thin, loose, hard, contain mucus, or even show blood depending on the severity of inflammation.
While some changes are mild and temporary, others require medical attention. Paying attention to your body and seeking help when needed ensures better digestive health and faster recovery.
If you notice persistent changes, especially with pain or fever, consult a healthcare professional. Knowing what’s normal—and what isn’t—gives you confidence and peace of mind.